Liliderm studies skin science and applies the science in all of its products. This section outlines the science behind the key active ingredients found within Liliderm products. Understanding the chemistry, the appropriate amounts, the proper mixture, and maximizing effectiveness is important to formulating and producing the best and most effective skin care products available.
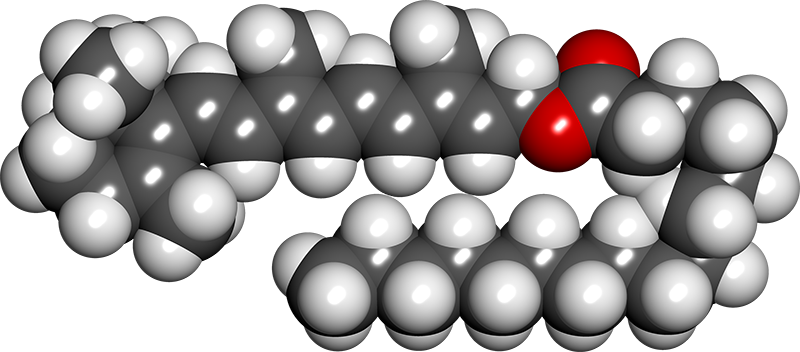
Retinyl Palmitate (Vitamin A)
Retinoids: active molecules influencing skin structure formation in cosmetic and dermatological treatments
Vitamin A is the first vitamin approved by the Food and Drug Administration as an anti-wrinkle agent that changes appearance of the skin surface and has anti-aging effects. Vitamin A is in a group of fat-soluble substances and belongs to the category of retinoids. Apart from retinol, that group includes structurally related substances with the biological properties of retinol. Since the biological activity of the substances differs, for the purpose of standardization, it is given in retinol equivalents. Vitamin A and its derivatives are among the most effective substances slowing the aging process. Retinoids regulate the cell apoptosis, differentiation and proliferation. Anti-wrinkle properties of retinoids promote keratinocytes proliferation, strengthen the protective function of the epidermis, restrain transepidermal water loss, protect collagen against degradation and inhibit metalloproteinases activity. Retinoid activity is related to high affinity for nuclear receptors: RAR – retinoid acid receptors and RXR – retinoid X receptors.
Topical Application of Retinyl Palmitate-Loaded Nanotechnology-Based Drug Delivery Systems for the Treatment of Skin Aging
The objective of this study was to perform a structural characterization and evaluate the in vitro safety profile and in vitro antioxidant activity of liquid crystalline systems (LCS) with and without retinyl palmitate (RP). LCS containing polyether functional siloxane (PFS) as a surfactant, silicon glycol copolymer (SGC) as oil phase, and water in the ratios 30 : 25 : 45 and 40 : 50 : 10 with (OLSv = RP-loaded opaque liquid system and TLSv = RP-loaded transparent liquid system, respectively) and without (OLS and TLS, respectively) RP were studied. Samples were characterized using polarized light microscopy (PLM) and rheology analysis. In vitro safety profile was evaluated using red cell hemolysis and in vitrocytotoxicity assays. In vitro antioxidant activity was performed by the DPPH method. PLM analysis showed the presence of lamellar LCS just to TLS. Regardless of the presence of RP, the rheological studies showed the pseudoplastic behavior of the formulations. The results showed that the incorporation of RP in LCS improved the safety profile of the drug. In vitro antioxidant activity suggests that LCS presented a higher capacity to maintain the antioxidant activity of RP. PFS-based systems may be a promising platform for RP topical application for the treatment of skin aging.
Retinoids in the treatment of skin aging: an overview of clinical efficacy and safety
Aging of skin is an intricate biological process consisting of two types. While intrinsic or chronological aging is an inevitable process, photoaging involves the premature aging of skin occurring due to cumulative exposure to ultraviolet radiation. Chronological and photoaging both have clinically differentiable manifestations. Various natural and synthetic retinoids have been explored for the treatment of aging and many of them have shown histological and clinical improvement, but most of the studies have been carried out in patients presenting with photoaged skin. Amongst the retinoids, tretinoin possibly is the most potent and certainly the most widely investigated retinoid for photoaging therapy. Although retinoids show promise in the treatment of skin aging, irritant reactions such as burning, scaling or dermatitis associated with retinoid therapy limit their acceptance by patients. This problem is more prominent with tretinoin and tazarotene whereas other retinoids mainly represented by retinaldehyde and retinol are considerably less irritating. In order to minimize these side effects, various novel drug delivery systems have been developed. In particular, nanoparticles have shown a good potential in improving the stability, tolerability and efficacy of retinoids like tretinoin and retinol. However, more elaborate clinical studies are required to confirm their advantage in the delivery of topical retinoids.
A comparative study of the effects of retinol and retinoic acid on histological, molecular, and clinical properties of human skin
All-trans retinol, a precursor of retinoic acid, is an effective anti-aging treatment widely used in skin care products. The results of this study demonstrate that topical application of retinol significantly affects both cellular and molecular properties of the epidermis and dermis, as shown by skin biopsy and noninvasive imaging analyses. Although the magnitude tends to be smaller, retinol induces similar changes in skin histology, and gene and protein expression as compared to retinoic acid application. These results were confirmed by the significant facial anti-aging effect observed in the retinol efficacy clinical study.
Molecular basis of retinol anti-aging properties in naturally aged human skin in vivo
Retinoic acid has been shown to improve the aged-appearing skin. However, less is known about the anti-aging effects of retinol (ROL, vitamin A), a precursor of retinoic acid, in aged human skin in vivo. This study aimed to investigate the molecular basis of retinol anti-aging properties in naturally aged human skin in vivo. Topical ROL shows remarkable anti-aging effects through three major types of skin cells: epidermal keratinocytes, dermal endothelial cells and fibroblasts. Topical ROL significantly increased epidermal thickness by stimulating keratinocytes proliferation and upregulation of c-Jun transcription factor. In addition to epidermal changes, topical ROL significantly improved dermal extracellular matrix (ECM) microenvironment; increasing dermal vascularity by stimulating endothelial cells proliferation and ECM production (type I collagen, fibronectin, and elastin) by activating dermal fibroblasts.
Improvement of naturally aged skin with vitamin A (retinol)
Topical retinol improves fine wrinkles associated with natural aging. Significant induction of glycosaminoglycan, which is known to retain substantial water, and increased collagen production are most likely responsible for wrinkle effacement. With greater skin matrix synthesis, retinol-treated aged skin is more likely to withstand skin injury and ulcer formation along with improved appearance.
The effect of a vitamin A palmitate and antioxidant-containing oil-based moisturizer on photodamaged skin of several body sites
Cumulative lifetime sun exposure is accepted as having a very important role to play in the expression of the signs of photoaging, which is then superimposed on the intrinsic processes involved in the chronological aging of skin. Collectively, these results show the cumulative improvements in the signs of photoaging compared to a no-treatment control group for the oil-based antiaging moisturizer for the first time. The differences in the efficacy of the vitamin A palmiate and antioxidant oil-based moisturizer on different body sites probably reflect the differences in likely photodamage.
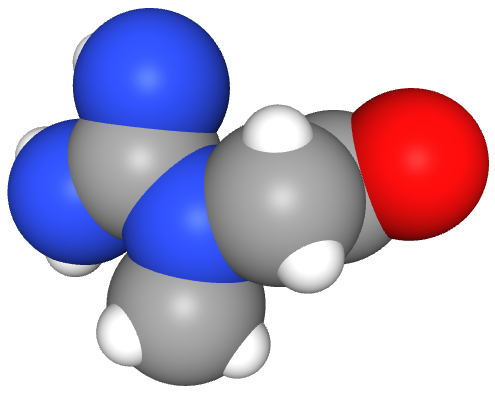
Niacinamide (Vitamin B3)
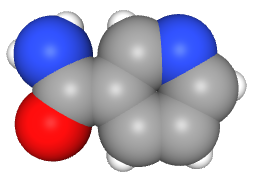
Niacinamide - mechanisms of action and its topical use in dermatology
Niacinamide, an amide of vitamin B3 (niacin), is a hydrophilic endogenous substance. Its effects after epicutaneous application have long been described in the literature. Given a sufficient bioavailability, niacinamide has antipruritic, antimicrobial, vasoactive, photo-protective, sebostatic and lightening effects depending on its concentration. Within a complex metabolic system niacinamide controls the NFκB-mediated transcription of signalling molecules by inhibiting the nuclear poly (ADP-ribose) polymerase-1 (PARP-1). Niacinamide is a well-tolerated and safe substance often used in cosmetics. Clinical data for its therapeutic use in various dermatoses can increasingly be found in the literature.
Nicotinic acid/niacinamide and the skin
Nicotinic acid (also generally known as niacin) and niacinamide (also known as nicotinamide) are similarly effective as a vitamin because they can be converted into each other within the organism. The blanket term vitamin B(3) is used for both. Niacinamide is a component of important coenzymes involved in hydrogen transfer. Topical application of niacinamide has a stabilizing effect on epidermal barrier function, seen as a reduction in transepidermal water loss and an improvement in the moisture content of the horny layer. Niacinamide leads to an increase in protein synthesis (e.g. keratin), has a stimulating effect on ceramide synthesis, speeds up the differentiation of keratinocytes, and raises intracellular NADP levels. In ageing skin, topical application of niacinamide improves the surface structure, smoothes out wrinkles and inhibits photocarcinogenesis. It is possible to demonstrate anti-inflammatory effects in acne, rosacea and nitrogen mustard-induced irritation. Because of its verifiable beneficial effects, niacinamide would be a suitable component in cosmetic products for use in disorders of epidermal barrier function, for ageing skin, for improving pigmentary disorders and for use on skin prone to acne.
Niacinamide: A B vitamin that improves aging facial skin appearance
In multiple chronic clinical studies, topical niacinamide (vitamin B3) has been observed to be well tolerated by skin and to provide a broad array of improvements in the appearance of aging facial skin (eg, reduction in the appearance of hyperpigmentated spots and red blotchiness). Analyses of the data revealed a variety of significant skin appearance improvement effects for topical niacinamide: reductions in fine lines and wrinkles, hyperpigmented spots, red blotchiness, and skin sallowness (yellowing). In addition, elasticity (as measured via cutometry) was improved.
A Double-Blind, Randomized Clinical Trial of Niacinamide 4% versus Hydroquinone 4% in the Treatment of Melasma
Background. Multiple modalities have been used in the treatment of melasma with variable success. Niacinamide has anti-inflammatory properties and is able to decrease the transfer of melanosomes. Objective. To evaluate the therapeutic effect of topical niacinamide versus hydroquinone (HQ) in melasma patients. Patients and Methods. Twenty-seven melasma patients were randomized to receive for eight weeks 4% niacinamide cream on one side of the face, and 4% HQ cream on the other. Sunscreen was applied along the observation period. They were assessed by noninvasive techniques for the evaluation of skin color, as well as subjective scales and histological sections initially and after the treatment with niacinamide. Results. All patients showed pigment improvement with both treatments. Colorimetric measures did not show statistical differences between both sides. However, good to excellent improvement was observed with niacinamide in 44% of patients, compared to 55% with HQ. Niacinamide reduced importantly the mast cell infiltrate and showed improvement of solar elastosis in melasma skin. Side effects were present in 18% with niacinamide versus 29% with HQ. Conclusion. Niacinamide induces a decrease in pigmentation, inflammatory infiltrate, and solar elastosis. Niacinamide is a safe and effective therapeutic agent for this condition.
Niacinamide Protects Skin Cells from Oxidative Stress Induced by Particulate Matter
Niacinamide (NIA) is a water-soluble vitamin that is widely used in the treatment of skin diseases. Moreover, NIA displays antioxidant effects and helps repair damaged DNA. Recent studies showed that particulate matter 2.5 (PM2.5) induced reactive oxygen species (ROS), causing disruption of DNA, lipids, and protein, mitochondrial depolarization, and apoptosis of skin keratinocytes. Here, we investigated the protective effects of NIA on PM2.5-induced oxidative stress in human HaCaT keratinocytes. We found that NIA could inhibit the ROS generation induced by PM2.5, as well block the PM2.5-induced oxidation of molecules, such as lipids, proteins, and DNA. Furthermore, NIA alleviated PM2.5-induced accumulation of cellular Ca2+, which caused cell membrane depolarization and apoptosis, and reduced the number of apoptotic cells. Collectively, the findings show that NIA can protect keratinocytes from PM2.5-induced oxidative stress and cell damage.
The effect of niacinamide on reducing cutaneous pigmentation and suppression of melanosome transfer
Cutaneous hyperpigmentation occurs in multiple conditions. Niacinamide gave 35-68% inhibition of melanosome transfer in the coculture model and reduced cutaneous pigmentation in the PREP model. In the clinical studies, niacinamide significantly decreased hyperpigmentation and increased skin lightness compared with vehicle alone after 4 weeks of use. The data suggest niacinamide is an effective skin lightening compound that works by inhibiting melanosome transfer from melanocytes to keratinocytes.
PANTOTHENIC ACID (Vitamin B5)
A Randomized, Double-Blind, Placebo-Controlled Study of a Novel Pantothenic Acid-Based Dietary Supplement in Subjects with Mild to Moderate Facial Acne
The results from this study indicate that the administration of a pantothenic acid-based dietary supplement in healthy adults with facial acne lesions is safe, well tolerated and reduced total facial lesion count versus placebo after 12 weeks of administration. Secondary analysis shows that the study agent significantly reduced area-specific and inflammatory blemishes.
Vitamin B5 (Pantothenic Acid)
Vitamin B5 is a medication used in the management and treatment of nutrient deficiencies. It is in the dietary supplement class of medications. This activity reviews the indications, actions, and contraindications for vitamin B5 as a valuable agent in treating nutritional deficiencies. This activity will highlight the mechanism of action, adverse event profile, and other key factors in the treatment of patients with nutritional deficiencies and related conditions.
Skin moisturizing effects of panthenol-based formulations
This study aims to evaluate the skin moisturizing efficacy of formulations containing different concentrations of panthenol. Formulations supplemented with or without 0.5%, 1.0%, or 5.0% panthenol were applied daily to the forearms of healthy subjects. Skin conditions in terms of moisture and transepidermal water loss (TEWL) were analyzed before and after 15- and 30-day periods of application. The formulations were also applied after skin washing with sodium laureth sulphate (SLES) to evaluate the immediate effects on TEWL and skin moisture. Panthenol-containing formulations (1.0% and 5.0%) produced significant decreases in TEWL after 30-day applications. In skin washed with SLES, significant reduction of TEWL was evident two hours after application of formulations loaded with panthenol when compared with control and vehicle. It is concluded that skin integrity is maintained by the improved protective effect of 1.0% panthenol added to the formulation.
Topical use of dexpanthenol in skin disorders
Pantothenic acid is essential to normal epithelial function. It is a component of coenzyme A, which serves as a cofactor for a variety of enzyme-catalyzed reactions that are important in the metabolism of carbohydrates, fatty acids, proteins, gluconeogenesis, sterols, steroid hormones, and porphyrins. The topical use of dexpanthenol, the stable alcoholic analog of pantothenic acid, is based on good skin penetration and high local concentrations of dexpanthenol when administered in an adequate vehicle, such as water-in-oil emulsions. Topical dexpanthenol acts like a moisturizer, improving stratum corneum hydration, reducing transepidermal water loss and maintaining skin softness and elasticity.
Dexpanthenol enhances skin barrier repair and reduces inflammation after sodium lauryl sulphate-induced irritation
Dexpanthenol-containing creams have been widely used for treatment of lesions (superficial wounds) of the skin and mucous membranes. Dexpanthenol is converted in tissues to pantothenic acid, a component of coenzyme A. Significantly accelerated skin barrier repair was found in treatments with the dexpanthenol-containing cream (verum) compared with vehicle-treated (placebo) or untreated skin.
Efficacy of dexpanthenol in skin protection against irritation: a double-blind, placebo-controlled study
Dexpanthenol is popular in treating various dermatoses and in skin care, but few controlled clinical trials have been performed. We investigated the efficacy of dexpanthenol in skin protection against irritation in a randomized, prospective, double-blind, placebo-controlled study. 25 healthy volunteers (age 18-45 years) were treated for the inner aspect of both forearms with either Bepanthol Handbalsam containing 5% dexpanthenol or placebo x2 daily for 26 days. From day 15-22, sodium lauryl sulfate (SLS) 2% was applied to these areas x2 daily. Documentation comprised sebumetry, corneometry, pH value and clinical appearance (photographs). 21 volunteers completed the study, 3 were excluded because of non-compliance and 1 experienced a non-study-related, severe, adverse event. Only corneometry yielded a statistically significant difference, with decreased values following SLS challenge at the placebo sites (P < 0.05). Intraindividual comparisons showed superior results at the dexpanthenol-treated sites in 11 cases and in only 1 case at the placebo site. 6 volunteers experienced an irritant contact dermatitis, with more severe symptoms at the placebo site in 5 cases. In conclusion, dexpanthenol exhibits protective effects against skin irritation. The initiation of a study to evaluate the efficacy of dexpanthenol in preventing irritant occupational contact dermatitis under real workplace conditions is validated.
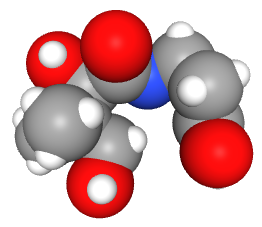
FOLIC ACID
Folic acid in general medicine and dermatology
Folic acid is a vitamin B essential for the integrity and function of DNA. Relative deficiency of folic acid may occur in conditions such as pregnancy and hyperproliferative or chronic inflammatory disorders. Folic acid supplementation appears as a reasonable therapeutic option in patients affected by chronic inflammatory skin diseases, such as moderate to severe psoriasis; in particular, those with concomitant hyperhomocysteinemia, low plasma folate and additional cardiovascular risk factors.
Folic acid and creatine improve the firmness of human skin in vivo
The decrease in firmness is a hallmark of skin aging. Accelerated by chronic sun exposure, fundamental changes occur within the dermal extracellular matrix over the years, mainly impairing the collagenous network. Employing MPLSM, dermal changes occurring in photo-aged human skin were visualized in an unprecedented manner and correlated to a loss of firmness. Treatment of aged skin with a topical formulation containing folic acid and creatine counteracted this age-dependent decline by exerting sustained effects on collagen metabolism. Our results support previous findings on the efficacy of these actives.
Folic Acid
Folic acid has FDA-approval for the treatment of megaloblastic and macrocytic anemias due to folic deficiency. Folic acid is a water-soluble vitamin used in the management and treatment of megaloblastic anemia. This activity describes the indications, mechanism of action, and contraindications for folic acid as a valuable agent in the management of megaloblastic anemia and the prevention of other disorders. This activity will highlight the adverse event profile and other key factors (e.g., off-label uses, dosing, monitoring, relevant interactions) pertinent for healthcare teams dealing with conditions that can benefit from folic acid.
L-ascorbic acid (Vitamin C)
Vitamin C in dermatology
Vitamin C is a potent antioxidant drug that can be used topically in dermatology to treat and prevent changes associated with photoageing. It can also be used for the treatment of hyperpigmentation. Because it is unstable and difficult to deliver into the dermis in the optimum dosage, research is being directed to find stable compounds of Vitamin C and newer methods of delivery of Vitamin C into the dermis.
Topical Vitamin C and the Skin: Mechanisms of Action and Clinical Applications
OBJECTIVE: This review article details the main mechanisms of action and clinical applications of topical vitamin C on the skin, including its antioxidative, photoprotective, antiaging, and antipigmentary effects. DESIGN: A PubMed search for the relevant articles on vitamin C and the skin was conducted using the following key words: “vitamin C,” “ascorbic acid,” “ascorbyl-6-palmitate,”and “magnesium ascorbyl phosphate.” RESULTS: As one of the most powerful antioxidants in the skin, vitamin C has been shown to protect against photoaging, ultraviolet-induced immunosuppression, and photocarcinogenesis. It also has an antiaging effect by increasing collagen synthesis, stabilizing collagen fibers, and decreasing collagen degradation. It decreases melanin formation, thereby reducing pigmentation. Vitamin C is the primary replenisher of vitamin E and works synergistically with vitamin E in the protection against oxidative damage. CONCLUSION: Topical vitamin C has a wide range of clinical applications, from antiaging and antipigmentary to photoprotective. Currently, clinical studies on the efficacy of topical formulations of vitamin C remain limited, and the challenge lies in finding the most stable and permeable formulation in achieving the optimal results.
The Roles of Vitamin C in Skin Health
The primary function of the skin is to act as a barrier against insults from the environment, and its unique structure reflects this. The skin is composed of two layers: the epidermal outer layer is highly cellular and provides the barrier function, and the inner dermal layer ensures strength and elasticity and gives nutritional support to the epidermis. Normal skin contains high concentrations of vitamin C, which supports important and well-known functions, stimulating collagen synthesis and assisting in antioxidant protection against UV-induced photodamage. This knowledge is often used as a rationale for the addition of vitamin C to topical applications, but the efficacy of such treatment, as opposed to optimising dietary vitamin C intake, is poorly understood. This review discusses the potential roles for vitamin C in skin health and summarises the in vitro and in vivo research to date. We compare the efficacy of nutritional intake of vitamin C versus topical application, identify the areas where lack of evidence limits our understanding of the potential benefits of vitamin C on skin health, and suggest which skin properties are most likely to benefit from improved nutritional vitamin C intake.
Double-blind, half-face study comparing topical vitamin C and vehicle for rejuvenation of photodamage
This formulation of vitamin C results in clinically visible and statistically significant improvement in wrinkling when used topically for 12 weeks. This clinical improvement correlates with biopsy evidence of new collagen formation.
Sun Role of Vitamin C in Skin Diseases
Vitamin C (ascorbic acid) plays an important role in maintaining skin health and can promote the differentiation of keratinocytes and decrease melanin synthesis, leading to antioxidant protection against UV-induced photodamage. Normal skin needs high concentrations of vitamin C, which plays many roles in the skin, including the formation of the skin barrier and collagen in the dermis, the ability to counteract skin oxidation, and the modulation of cell signal pathways of cell growth and differentiation. However, vitamin C deficiency can cause or aggravate the occurrence and development of some skin diseases, such as atopic dermatitis (AD) and porphyria cutanea tarda (PCT). Levels of vitamin C in plasma are decreased in AD, and vitamin C deficiency may be one of the factors that contributes to the pathogenesis of PCT. On the other hand, high doses of vitamin C have significantly reduced cancer cell viability, as well as invasiveness, and induced apoptosis in human malignant melanoma. In this review, we will summarize the effects of vitamin C on four skin diseases (porphyria cutanea tarda, atopic dermatitis, malignant melanoma, and herpes zoster and postherpetic neuralgia) and highlight the potential of vitamin C as a therapeutic strategy to treat these diseases, emphasizing the clinical application of vitamin C as an adjuvant for drugs or physical therapy in other skin diseases.
The role of vitamin C in pushing back the boundaries of skin aging: an ultrasonographic approach
Our study shows that topically applied vitamin C is highly efficient as a rejuvenation therapy, inducing significant collagen synthesis in all age groups with minimal side effects.
Split-face study of topical 23.8% L-ascorbic acid serum in treating photo-aged skin
Topical 23.8% L-ascorbic acid serum is effective for the treatment of photo-aged skin and does not cause any obvious side effects.
Topical ascorbic acid on photoaged skin. Clinical, topographical and ultrastructural evaluation: double-blind study vs. placebo
Vitamin C is known for its antioxidant potential and activity in the collagen biosynthetic pathway. Photoprotective properties of topically applied vitamin C have also been demonstrated, placing this molecule as a potential candidate for use in the prevention and treatment of skin ageing. Topical application of 5% vitamin C cream was an effective and well-tolerated treatment. It led to a clinically apparent improvement of the photodamaged skin and induced modifications of skin relief and ultrastructure, suggesting a positive influence of topical vitamin C on parameters characteristic for sun-induced skin ageing.
The effect of Vitamin C on melanin pigmentation – A systematic review
Vitamin C, also known as ascorbic acid, is used as a treatment modality in depigmentation of hyperpigmented spots on the skin and gingiva. This systematic review discusses the studies conducted to assess the effect of Vitamin C on melanin pigmentation. The primary objective was to evaluate the effect of Vitamin C on melanin pigmentation. The secondary objective was to analyze the effect of Vitamin C administration on melanin pigmentation. An electronic database search was conducted from the following databases: PubMed, EBSCOhost, ScienceOpen, EMBASE and Google Scholar. Randomized controlled trials, experimental studies, case–control studies and cohort studies published in peer-reviewed journals in English language were included. Case reports, case series, animal model studies, in vitro studies, studies where Vitamin C was used along with other agents and unpublished research were excluded. Out of 22,580 studies, only 7 studies satisfied the selection criteria. Data extraction sheet was prepared, and the studies were analyzed. Out of the 7 studies analyzed, 1 was a randomized controlled trial and 6 were experimental studies. Vitamin C has been used widely as a depigmenting agent in dermatology. However, there are limited studies conducted on the use of Vitamin C for gingival depigmentation.
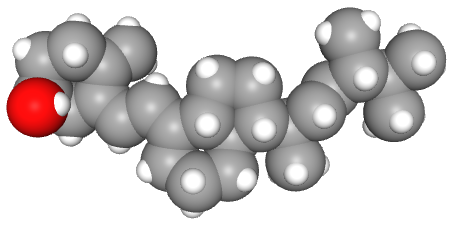
Ɑ-Tocopherol (Vitamin E)
Vitamin E in dermatology
Vitamin E is an important fat-soluble antioxidant and has been in use for more than 50 years in dermatology. It is an important ingredient in many cosmetic products. It protects the skin from various deleterious effects due to solar radiation by acting as a free-radical scavenger. Experimental studies suggest that vitamin E has antitumorigenic and photoprotective properties. There is a paucity of controlled clinical studies providing a rationale for well-defined dosages and clinical indications of vitamin E usage in dermatological practice. The aim of this article is to review the cosmetic as well as clinical implications of vitamin E in dermatology.
Vitamin E in dermatology
Vitamin E is an important fat-soluble antioxidant and has been in use for more than 50 years in dermatology. It is an important ingredient in many cosmetic products. It protects the skin from various deleterious effects due to solar radiation by acting as a free-radical scavenger. Experimental studies suggest that vitamin E has antitumorigenic and photoprotective properties. There is a paucity of controlled clinical studies providing a rationale for well-defined dosages and clinical indications of vitamin E usage in dermatological practice.
Antioxidants in dermatology
The skin cells continuously produce, through cellular respiration, metabolic processes or under external aggressions, highly reactive molecules oxidation products, generally called free radicals. These molecules are immediately neutralized by enzymatic and non-enzymatic systems in a physiological and dynamic balance. In situations where this balance is broken, various cellular structures, such as the cell membrane, nuclear or mitochondrial DNA may suffer structural modifications, triggering or worsening skin diseases. several substances with alleged antioxidant effects has been offered for topical or oral use, but little is known about their safety, possible associations and especially their mechanism of action. The management of topical and oral antioxidants can help dermatologist to intervene in the oxidative processes safely and effectively, since they know the mechanisms, limitations and potential risks of using these molecules as well as the potential benefits of available associations.
Biological and Pharmacological Activities of Squalene and Related Compounds: Potential Uses in Cosmetic Dermatology
Vitamin E is a group of eight different compounds, but only two of the forms, α-tocopherol and γ-tocopherol, are commonly found in the human body [44]. Lopez-Torres et al. [46] investigated the effects of topical α-tocopherol application on epidermal and dermal tissues and its ability to prevent UV-induced oxidative damage. Hairless mice received a topical application of α-tocopherol 24 h before a single acute exposure to UV irradiation (10 × minimal erythemal dose). α-Tocopherol treatment significantly reduced the formation of epidermal lipid hydroperoxides after UV irradiation (p < 0.05). Those results demonstrated that topical administration of α-tocopherol protects cutaneous tissues against oxidative damage induced by UV irradiation in vivo.
Clinical evaluation of photoprotective effect by a topical antioxidants combination (tocopherols and tocotrienols)
The use of a new topical formulation containing significant concentrations of tocotrienols and tocopherols represents a promising strategy to reduce the photo-induced skin damage.
UV photoprotection by combination topical antioxidants vitamin C and vitamin E
Virtually all plants and animals protect themselves from the sun using vitamins C and E. Appreciable photoprotection can be obtained from the combination of topical vitamins C and E. We suggest that these natural products may protect against skin cancer and photoaging.
Zinc (zinc oxide)
Zinc Therapy in Dermatology: A Review
Zinc, both in elemental or in its salt forms, has been used as a therapeutic modality for centuries. Topical preparations like zinc oxide, calamine, or zinc pyrithione have been in use as photoprotecting, soothing agents or as active ingredient of antidandruff shampoos. Its use has expanded manifold over the years for a number of dermatological conditions including infections (leishmaniasis, warts), inflammatory dermatoses (acne vulgaris, rosacea), pigmentary disorders (melasma), and neoplasias (basal cell carcinoma). Although the role of oral zinc is well-established in human zinc deficiency syndromes including acrodermatitis enteropathica, it is only in recent years that importance of zinc as a micronutrient essential for infant growth and development has been recognized. The paper reviews various dermatological uses of zinc.
Skin-protective effects of a zinc oxide-functionalized textile and its relevance for atopic dermatitis
Atopic dermatitis (AD) is a chronic inflammatory disease characterized by the impairment of the skin-barrier function, increased oxidative cellular stress, and bacterial colonization. Hence, medical therapies of AD aim to control infection, reduce inflammation, and restore skin-barrier function by use of topical and systemic antibacterial drugs, topical corticosteroids, topical calcineurin inhibitors, and moisturizers. Textiles have the longest and most intense contact with the human skin, and functional textiles with intrinsic properties such as antioxidative capacity and antibacterial activity have been gaining in importance in medical applications. Specially designed textiles may support AD treatment and improve quality of life of AD. Here, we investigated the role of ZnO-functionalized textile fibers in the control of oxidative stress in AD in vitro and in vivo. In addition, the antibacterial effect and biocompatibility of the Zn textile was evaluated in vitro. We observed a rapid improvement of AD severity, pruritus, and subjective sleep quality when AD patients wore the ZnO textiles overnight on 3 consecutive days. This is possibly due to the high antioxidative capacity of the ZnO textile, as well as the allocation of strong antibacterial activity. Moreover, it was shown that the ZnO textiles possess very good biocompatibility and were well tolerated by AD patients.
Innovative uses for zinc in dermatology
Severe zinc deficiency states, such as acrodermatitis enteropathica, are associated with a variety of skin manifestations, such as perioral, acral, and perineal dermatitis. These syndromes can be reversed with systemic zinc repletion. In addition to skin pathologies that are clearly zinc-dependent, many dermatologic conditions (eg, dandruff, acne, and diaper rash) have been associated and treated with zinc. Success rates for treatment with zinc vary greatly depending on the disease, mode of administration, and precise zinc preparation used. With the exception of systemic zinc deficiency states, there is little evidence that convincingly demonstrates the efficacy of zinc as a reliable first-line treatment for most dermatologic conditions. However, zinc may be considered as an adjunctive treatment modality. Further research is needed to establish the indications for zinc treatment in dermatology, optimal mode of zinc delivery, and best type of zinc compound to be used.
Zinc oxide nanoparticles: a 90-day repeated-dose dermal toxicity study in rats
Zinc oxide (ZnO) works as a long-lasting, broad-spectrum physical sunblock, and can prevent skin cancer, sunburn, and photoaging. Nanosized ZnO particles are used often in sunscreens due to consumer preference over larger sizes, which appear opaque when dermally applied. This study demonstrates that there was no observed adverse effect of ZnO NPs up to 1,000 mg/kg body weight when they are applied dermally.
Zinc in Wound Healing Modulation
Wound care is a major healthcare expenditure. Treatment of burns, surgical and trauma wounds, diabetic lower limb ulcers and skin wounds is a major medical challenge with current therapies largely focused on supportive care measures. Successful wound repair requires a series of tightly coordinated steps including coagulation, inflammation, angiogenesis, new tissue formation and extracellular matrix remodelling. Zinc is an essential trace element (micronutrient) which plays important roles in human physiology. Zinc is a cofactor for many metalloenzymes required for cell membrane repair, cell proliferation, growth and immune system function. The pathological effects of zinc deficiency include the occurrence of skin lesions, growth retardation, impaired immune function and compromised would healing. Here, we discuss investigations on the cellular and molecular mechanisms of zinc in modulating the wound healing process. Knowledge gained from this body of research will help to translate these findings into future clinical management of wound healing.
The clinical effects of zinc as a topical or oral agent on the clinical response and pathophysiologic mechanisms of acne: a systematic review of the literature
This article reviews the published literature about the efficacy of oral and topical zinc as treatments for acne vulgaris. The medical literature was systematically reviewed to identify relevant articles. Each published study was assessed for pathophysiologic results and the quality of the clinical evidence the study provided based on Strength of Recommendation Taxonomy (SORT) criteria. Finally, the body of evidence for using oral or topical zinc in the treatment of acne was assessed, again using SORT criteria. A SORT strength of recommendation of B (inconsistent or limited-quality patient-oriented evidence) appears to be appropriate for both oral and topical zinc. The preponderance of evidence suggests zinc has antibacterial and anti-inflammatory effects and that it may decrease sebum production.
Caffeine
Caffeine's mechanisms of action and its cosmetic use
Caffeine is being increasingly used in cosmetics due to its high biological activity and ability to penetrate the skin barrier. This alkaloid is frequently used as a hydrophilic model substance in human and animal skin penetration as well as different synthetic membrane using Franz diffusion cell experiments. The commercially available topical formulations of caffeine normally contain 3% caffeine. As for a cosmetic purpose, caffeine is used as an active compound in anti-cellulite products because it prevents excessive accumulation of fat in cells. This alkaloid stimulates the degradation of fats during lipolysis through inhibition of the phosphodiesterase activity. Caffeine has potent antioxidant properties. It helps protect cells against the UV radiation and slows down the process of photoaging of the skin.
Caffeine Protects Skin from Oxidative Stress-Induced Senescence through the Activation of Autophagy
Skin cells are vulnerable to oxidative stress-induced senescence, which may lead to abnormal aging or aging-related disorders. Therefore, strategies that can ameliorate oxidative stress-induced senescence are expected to protect skin from damage, holding the promise of treating skin diseases in the clinic. The results reveal that caffeine protects skin from oxidative stress-induced senescence through activating the A2AR/SIRT3/AMPK-mediated autophagy. Our study not only demonstrated the beneficial effect of caffeine using both in vitro and in vivo models, but also systematically investigated the underlying molecular mechanisms. These discoveries implicate the potential of caffeine in the protection of skin disease.
Histopathological evaluation of caffeine-loaded solid lipid nanoparticles in efficient treatment of cellulite
Cellulite refers to dimpled appearance of the skin, usually located in the thighs and buttocks regions of most adult women. Results of this study indicated that SLNs are promising carrier for improvement of caffeine efficiency in the treatment of cellulite following topical application on the skin.
Linoleic acid
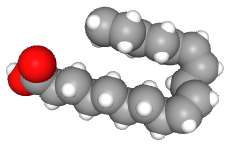
Healing fats of the skin: the structural and immunologic roles of the omega-6 and omega-3 fatty acids
Linoleic acid (18:2omega6) and alpha-linolenic acid (18:3omega3) represent the parent fats of the two main classes of polyunsaturated fatty acids: the omega-6 (n-6) and the omega-3 (n-3) fatty acids, respectively. Linoleic acid and alpha-linolenic acid both give rise to other long-chain fatty acid derivatives, including gamma-linolenic acid and arachidonic acid (omega-6 fatty acids) and docosahexaenoic acid and eicosapentaenoic acid (omega-3 fatty acids). These fatty acids are showing promise as safe adjunctive treatments for many skin disorders, including atopic dermatitis, psoriasis, acne vulgaris, systemic lupus erythematosus, nonmelanoma skin cancer, and melanoma. Their roles are diverse and include maintenance of the stratum corneum permeability barrier, maturation and differentiation of the stratum corneum, formation and secretion of lamellar bodies, inhibition of proinflammatory eicosanoids, elevation of the sunburn threshold, inhibition of proinflammatory cytokines (tumor necrosis factor-alpha, interferon-gamma, and interleukin-12), inhibition of lipoxygenase, promotion of wound healing, and promotion of apoptosis in malignant cells, including melanoma. They fulfill these functions independently and through the modulation of peroxisome proliferator-activated receptors and Toll-like receptors.
Comparison of linoleic acid-containing water-in-oil emulsion with urea-containing water-in-oil emulsion in the treatment of atopic dermatitis: a randomized clinical trial
Application of topical moisturizers is an essential part of the management of atopic dermatitis (AD). Linoleic acid (LA), the most abundant fatty acid in the epidermis, and its derivatives have an essential role in the structure and function of the epidermal barrier, and their defects are prominent in AD. Both LA- or urea-containing w/o emulsions can significantly improve barrier dysfunction and clinical severity of AD. In agreement with literature, it was confirmed that an LA-containing w/o emulsion exhibited erythema-reducing effects.
Cosmetic and Therapeutic Applications of Fish Oil’s Fatty Acids on the Skin
Fish oil has been broadly reported as a potential supplement to ameliorate the severity of some skin disorders such as photoaging, skin cancer, allergy, dermatitis, cutaneous wounds, and melanogenesis. Fish oil and the related actives, such as omega-3 and omega-6 PUFAs, have been proved helpful for maintaining skin homeostasis and ameliorating cutaneous abnormalities. The fatty acids in fish oil can improve skin barrier function, inhibit UV-induced inflammation and hyperpigmentation, attenuate dry skin and pruritus elicited by dermatitis, accelerate skin wound healing, and prevent skin cancer development. All the benefits can be achieved by different administration routes, including oral supplementation, topical application, and intravenous injection. Another issue that should be considered is that not only PUFAs but also vitamin A, vitamin D, retinol, selenium, and other components may contribute to the bioactivity of fish oil.
Linoleic acid also imparts anti-inflammatory properties through conversion to arachidonic acid, which leads to prostaglandin E2 (PGE2), possibly via peroxisome proliferative-activated receptor-a (PPAR-a) activation. PGE2 suppresses T cell receptor signaling and may play a role in resolution of inflammation. PPAR-a activation also enhances keratinocyte proliferation and lipid synthesis. This in turn enhances skin barrier repair.
There is also research that suggests linoleic acid may possess acne reductive properties. It has been hypothesized that a relative decrease in linoleic acid in the sebum (the skin’s natural oil) could contribute to the formation of acne. A study published in Clinical and Experimental Dermatology evaluated the effects of topically applied linoleic acid on the size of microcomedones in patients with mild acne. After a one month treatment period, there was a significant effect of topically applied linoleic acid on the size of microcomedones, an almost 25% reduction in their overall size.
Linoleic acid has also been studied for its skin-lightening effects. Studies have found that linoleic can lighten dark spots on the skin due to suppression of melanin production by active melanocytes. Melanocytes are cells within the epidermis that produce melanin, the pigment that gives our skin color. Excessive melanin production, caused by factors such as UV exposure, inflammatory conditions, acne, and injuries to the skin, can lead to uneven skin tone and dark spots. Thus, by inhibiting melanin production, linoleic acid helps to lighten skin and even out the skin tone.
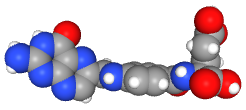
HYALURONIC ACID
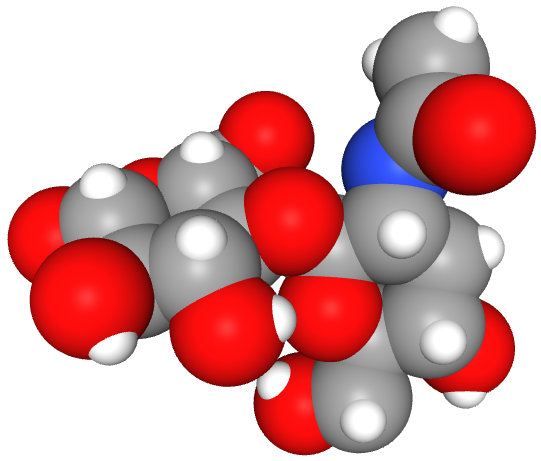
Hyaluronic acid: A key molecule in skin aging
Skin aging is a multifactorial process consisting of two distinct and independent mechanisms: intrinsic and extrinsic aging. Youthful skin retains its turgor, resilience and pliability, among others, due to its high content of water. Daily external injury, in addition to the normal process of aging, causes loss of moisture. The key molecule involved in skin moisture is hyaluronic acid (HA) that has unique capacity in retaining water. There are multiple sites for the control of HA synthesis, deposition, cell and protein association and degradation, reflecting the complexity of HA metabolism. The enzymes that synthesize or catabolize HA and HA receptors responsible for many of the functions of HA are all multigene families with distinct patterns of tissue expression. Understanding the metabolism of HA in the different layers of the skin and the interactions of HA with other skin components will facilitate the ability to modulate skin moisture in a rational manner.
Hyaluronic Acid: Molecular Mechanisms and Therapeutic Trajectory
Hyaluronic acid (also known as hyaluronan or hyaluronate) is naturally found in many tissues and fluids, but more abundantly in articular cartilage and synovial fluid (SF). Hyaluronic acid (HA) content varies widely in different joints and species. HA is a non-sulfated, naturally occurring non-protein glycosaminoglycan (GAG), with distinct physico-chemical properties, produced by synoviocytes, fibroblasts, and chondrocytes. HA has an important role in the biomechanics of normal SF, where it is partially responsible for lubrication and viscoelasticity of the SF. The concentration of HA and its molecular weight (MW) decline as osteoarthritis (OA) progresses with aging. For that reason, HA has been used for more than four decades in the treatment of OA in dogs, horses and humans. HA produces anti-arthritic effects via multiple mechanisms involving receptors, enzymes and other metabolic pathways. HA is also used in the treatment of ophthalmic, dermal, burns, wound repair, and other health conditions. The MW of HA appears to play a critical role in the formulation of the products used in the treatment of diseases. This review provides a mechanism-based rationale for the use of HA in some disease conditions with special reference to OA.
Hyaluronic acid, a promising skin rejuvenating biomedicine: A review of recent updates and pre-clinical and clinical investigations on cosmetic and nutricosmetic effects
Hyaluronic acid (HA) plays multifaceted role in regulating the various biological processes such as skin repairmen, diagnosis of cancer, wound healing, tissue regeneration, anti-inflammatory, and immunomodulation. Owing to its remarkable biomedical and tissue regeneration potential, HA has been numerously employed as one of the imperative components of the cosmetic and nutricosmetic products. The present review aims to summarize and critically appraise recent developments and clinical investigations on cosmetic and nutricosmetic efficacy of HA for skin rejuvenation. A thorough analysis of the literature revealed that HA based formulations (i.e., gels, creams, intra-dermal filler injections, dermal fillers, facial fillers, autologous fat gels, lotion, serum, and implants, etc.) exhibit remarkable anti-wrinkle, anti-nasolabial fold, anti-aging, space-filling, and face rejuvenating properties. This has been achieved via soft tissue augmentation, improved skin hydration, collagen and elastin stimulation, and face volume restoration. HA, alone or in combination with lidocaine and other co-agents, showed promising efficacy in skin tightness and elasticity, face rejuvenation, improving aesthetic scores, reducing the wrinkle scars, longevity, and tear trough rejuvenation. Our critical analysis evidenced that application/administration of HA exhibits outstanding nutricosmetic efficacy and thus is warranted to be used as a prime component of cosmetic products.
CREATINE
The creatine kinase system in human skin: protective effects of creatine against oxidative and UV damage in vitro and in vivo
Cutaneous aging is characterized by a decline in cellular energy metabolism, which is mainly caused by detrimental changes in mitochondrial function. The processes involved seem to be predominantly mediated by free radicals known to be generated by exogenous noxes, e.g., solar ultraviolet (UV) radiation. Basically, skin cells try to compensate any loss of mitochondrial energetic capacity by extra-mitochondrial pathways such as glycolysis or the creatine kinase (CK) system. Recent studies reported the presence of cytosolic and mitochondrial isoenzymes of CK, as well as a creatine transporter in human skin. In this study, we analyzed the cutaneous CK system, focusing on those cellular stressors known to play an important role in the process of skin aging. According to our results, a stress-induced decline in mitochondrial energy supply in human epidermal cells correlated with a decrease in mitochondrial CK activity. In addition, we investigated the effects of creatine supplementation on human epidermal cells as a potential mechanism to reinforce the endogenous energy supply in skin. Exogenous creatine was taken up by keratinocytes and increased CK activity, mitochondrial function and protected against free oxygen radical stress. Finally, our new data clearly indicate that human skin cells that are energetically recharged with the naturally occurring energy precursor, creatine, are markedly protected against a variety of cellular stress conditions, like oxidative and UV damage in vitro and in vivo. This may have further implications in modulating processes, which are involved in premature skin aging and skin damage.
Folic acid and creatine improve the firmness of human skin in vivo
The underlying structural changes in the collagen network of young and aged sun-exposed facial skin in vivo were visualized by MPLSM. Topical application of a folic acid- and creatine-containing formulation significantly improved firmness of mature skin in vivo. Treatment of fibroblast-populated dermal equivalents with folic acid and creatine increased collagen gene expression and procollagen levels and improved collagen fiber density, suggesting that the in vivo effects are based on the overall improvement of the collagen metabolism.
VITAMIN D
Effect of vitamin D supplementation on testosterone levels in men
The male reproductive tract has been identified as a target tissue for vitamin D, and previous data suggest an association of 25-hydroxyvitamin D [25(OH)D] with testosterone levels in men. We therefore aimed to evaluate whether vitamin D supplementation influences testosterone levels in men. Healthy overweight men undergoing a weight reduction program who participated in a randomized controlled trial were analyzed for testosterone levels. Our results suggest that vitamin D supplementation might increase testosterone levels. Further randomized controlled trials are warranted to confirm this hypothesis.
Ergocalciferol promotes in vivo differentiation of keratinocytes and reduces photodamage caused by ultraviolet irradiation in hairless mice
Topical application of VD(2) significantly prevented wrinkle formation and abnormal accumulation of extracellular matrix components. In addition, VD(2) suppressed excessive secretion of IL-6 induced by UV irradiation in cultured human normal keratinocytes, in a dose-dependent manner. VD(2) promoted keratinocytes differentiation in the epidermis and showed diverse physiological effects, the same as the active form of VD(3). The results suggested that the suppression of skin photodamage involved the promotion of keratinocytes differentiation and suppression of IL-6 secretion induced by exposure to UV. Topical application of VD(2) may become an effective means to suppress solar UV-induced human skin damage.
Topical Delivery of Vitamin D3: A Randomized Controlled Pilot Study
In 50 female Medical students, this study was conducted. Age, weight and height was taken, a detailed history and clinical examination was performed. Blood was drawn for 25 Hydroxy Vitamin D3 (25OHD) level. Two women had >30 ng/mL of 25OHD and was excluded from the study. The participants were divided into two groups of 24 in each arm. The study group of women were asked to apply; Top-D (Aloe Vera based- Vitamin D3) (Patency Pending) was developed at King Fahd Hospital of the University, AlKhobar with each gram of the Top-D cream delivering 5000 IU of vitamin D3. The second group used 1 gram of Aloe vera gel. The participants had no knowledge to which group they belong. A second blood sample was taken at the end of 3 months and the data was analyzed. This randomized control study shows that vitamin D3 can safely be delivered through the dermal route. This route could be exploited in treating vitamin D deficiency.
MAGNESIUM
The Interplay between Magnesium and Testosterone in Modulating Physical Function in Men
The role of nutritional status as key factor of successful aging is very well recognized. Among the different mechanisms by which nutrients may exert their beneficial effects is the modulation of the hormonal anabolic milieu, which is significantly reduced with aging. Undernutrition and anabolic hormonal deficiency frequently coexist in older individuals determining an increased risk of mobility impairment and other adverse outcomes. Mineral assessment has received attention as an important determinant of physical performance. In particular, there is evidence that magnesium exerts a positive influence on anabolic hormonal status, including Testosterone, in men. In this review we summarize data from observational and intervention studies about the role of magnesium in Testosterone bioactivity and the potential underlying mechanisms of this relationship in male subjects. If larger studies will confirm these pivotal data, the combination of hormonal and mineral replacements might be adopted to prevent or delay the onset of disability in the elderly.
Bathing in a magnesium-rich Dead Sea salt solution improves skin barrier function, enhances skin hydration, and reduces inflammation in atopic dry skin
Magnesium salts, the prevalent minerals in Dead Sea water, are known to exhibit favorable effects in inflammatory diseases. We examined the efficacy of bathing atopic subjects in a salt rich in magnesium chloride from deep layers of the Dead Sea (Mavena(R) Dermaline Mg(46) Dead Sea salt, Mavena AG, Belp, Switzerland). Volunteers with atopic dry skin submerged one forearm for 15 min in a bath solution containing 5% Dead Sea salt. The second arm was submerged in tap water as control. Before the study and at weeks 1-6, transepidermal water loss (TEWL), skin hydration, skin roughness, and skin redness were determined. Skin hydration was enhanced on the forearm treated with the Dead Sea salt in each group, which means the treatment moisturized the skin. Skin roughness and redness of the skin as a marker for inflammation were significantly reduced after bathing in the salt solution. This demonstrates that bathing in the salt solution was well tolerated, improved skin barrier function, enhanced stratum corneum hydration, and reduced skin roughness and inflammation. We suggest that the favorable effects of bathing in the Dead Sea salt solution are most likely related to the high magnesium content. Magnesium salts are known to bind water, influence epidermal proliferation and differentiation, and enhance permeability barrier repair.

